Anti Reflux Surgery
What is Gastric Reflux?
Gastric reflux, also known as gastro-oesophageal reflux disease (GORD) or acid reflux, is a common medical condition that affects the digestive system. It occurs when stomach acid flows back into the oesophagus, the tube that connects your mouth to your stomach. This backflow of acid can lead to a range of symptoms and potential complications.
Causes of Gastric Reflux
Understanding the underlying factors contributing to this condition can help in its management. Here are some common causes:
- Weakened Lower Oesophageal Sphincter (LOS)
- Hiatal Hernia
- Dietary Factors
- Obesity
- Pregnancy
- Smoking
- Certain Medications (such as antihistamines, calcium channel blockers, and certain asthma medications)
- Stress
Impact of Gastric Reflux
Living with gastric reflux is inconvenient as symptoms can severely interfere with your life. You may be restricted in what you can eat, and reflux occurring in the night can hinder a good night's sleep, thereby affecting alertness and productivity the next day.
Symptoms of Gastric Reflux
Heartburn is usually the main symptom of GORD, characterised by a burning-type pain in the lower part of the mid-chest, behind the breastbone.
Other symptoms include:
- a bitter or sour taste in the mouth
- trouble swallowing
- nausea
- dry cough or wheezing
- regurgitation of food
- hoarseness or change in voice
- chest pain
Diagnosis for Gastric Reflux
Your surgeon may order some of the following tests to diagnose gastric reflux:
- Gastroscopy: Allows examination of the inside of your oesophagus, stomach and portions of the intestine with an instrument called an endoscope, a thin, flexible telescope. This is done in the hospital under anaesthesia.
- 24-hour pH monitoring: Involves inserting a tube through your nose into the oesophagus and positioning it above the LOS. The tube tip contains a sensor that can measure the pH of the acid content refluxed into the oesophagus. The tube will be left in place for 24 hours.
- Oesophageal Manometry: A tube placed into the oesophagus measures how well the muscles of the oesophagus work, which helps assess the problem.
- BRAVO capsule: This is an alternative way to measure acid exposure in the oesophagus. A small wireless capsule is introduced into the oesophagus using a gastroscope. The pH sensor transmits signals to a computer that collects the data about the acid exposure over the next 24 hours. The capsule eventually falls off the oesophagus lining and is safely passed in the stool.
Treatment Options for Gastric Reflux
Treatment aims to reduce reflux, relieve symptoms and prevent damage to the oesophagus. Some of the treatment options include:
- Antacids: Over-the-counter medicines that provide temporary relief to heartburn and indigestion by neutralising acid in the stomach. This is not usually an effective long-term option.
- Proton Pump Inhibitors: PPI drugs reduce the production of acid in the stomach
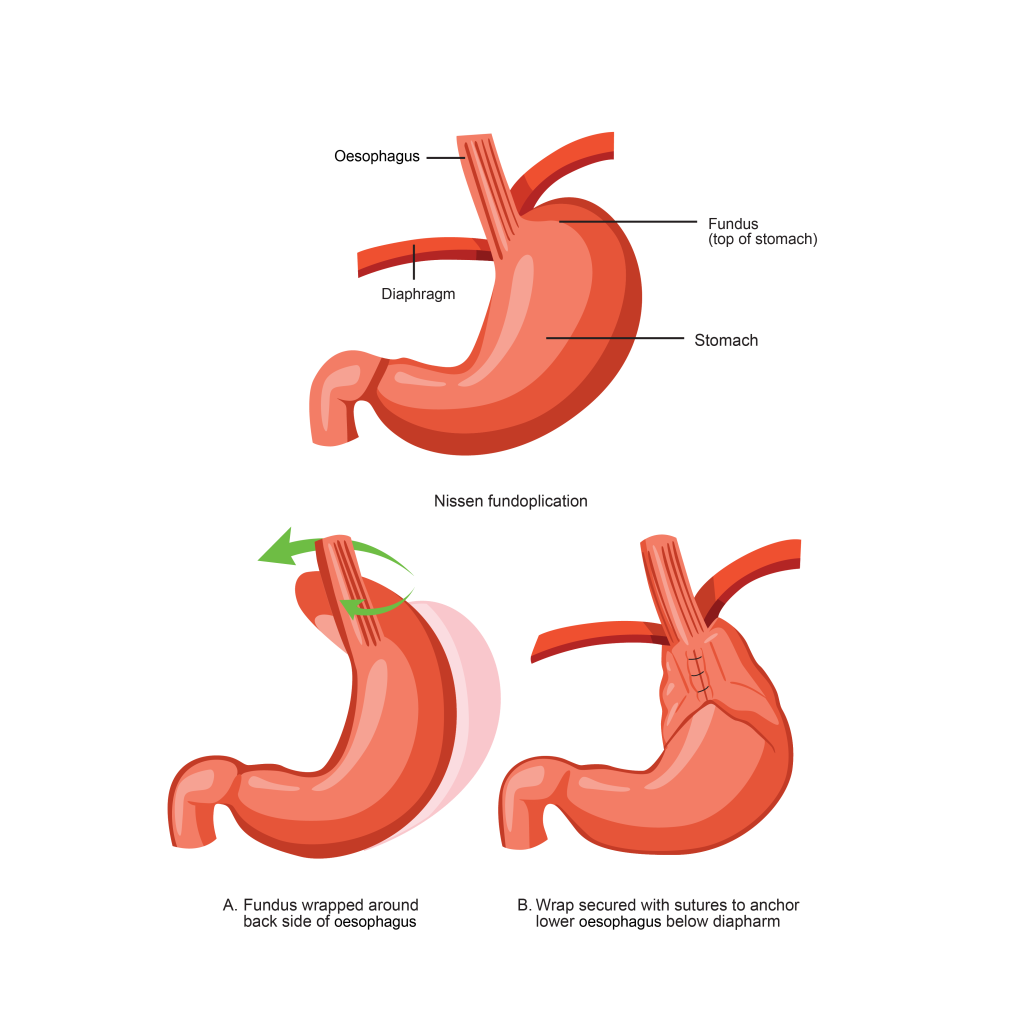
- Fundoplication/hiatus hernia repair: A key-hole surgical procedure in which the upper part of the stomach is wrapped around the lower end of your oesophagus, where it is sutured into place. If there is a weakness in the diaphragm, this is repaired also. This surgery helps prevent stomach acid and food from flowing back into the oesophagus.
What is Anti Reflux Surgery?
Anti-reflux surgery, or fundoplication, is a surgical procedure used to treat gastro-oesophageal reflux disease (GORD). During this surgery, the upper part of the stomach is wrapped around the lower oesophagus, creating a valve-like mechanism that prevents stomach acid from flowing back up.
Who is a Candidate for Anti-Reflux Surgery?
- Individuals with severe GORD who are not adequately controlled with medications.
- Patients who experience frequent regurgitation or heartburn, even on medication.
- Patients who have a preference for not being on medications in the long term.
- People with complications from GORD, such as oesophageal ulcerations or Barrett's oesophagus.
Benefits of Anti-Reflux Surgery
Anti-reflux surgery offers several benefits for individuals with chronic GORD, including:
- Relief from GORD Symptoms: Alleviate symptoms such as heartburn, regurgitation, chest pain, and difficulty swallowing, providing significant relief and improving quality of life.
- Reduced Medication Dependence: For individuals who rely on long-term medication to manage GORD, surgery may reduce or eliminate the need for daily medication, offering a more sustainable solution.
- Improved Oesophageal Health: By preventing the backward flow of stomach acid into the oesophagus, anti-reflux surgery can help prevent complications such as esophageal inflammation ulcers and likely reduce the chances of developing premalignant changes or cancer of the oesophagus.
Types of Anti-Reflux Surgery
There are different types of anti-reflux surgery procedures available, including:
- Nissen Fundoplication: This is a common type of surgery performed for hiatus hernia repair. It involves wrapping the upper part of the stomach (fundus) around the lower oesophagus to strengthen the lower esophageal sphincter and prevent acid reflux.
- Toupet Fundoplication: A partial wrap procedure that addresses the hernia while preserving the ability to swallow effectively. It involves wrapping only a portion of the stomach around the ¾ of the lower oesophagus.
- Dor Fundoplication: A partial wrap procedure that addresses the hernia while preserving the ability to swallow effectively. It involves wrapping only a portion of the stomach around ½ of the lower oesophagus.
- Weight loss surgery: Reflux in patients with obesity is a significant and common problem. Often, a weight loss operation can help with obesity-causing reflux and also create a low-pressure system to prevent reflux from recurring.
Alternative Options for Anti-Reflux Surgery
In addition to anti-reflux surgery, alternative treatment options are available for managing GORD. These may include:
- Medication: Prescription and over-the-counter medications, such as proton pump inhibitors (PPIs) and H2 receptor blockers, can help reduce stomach acid production and alleviate GORD symptoms. However, they provide temporary relief and may not address the underlying cause.
- Lifestyle Modifications: This may involve weight loss, avoiding trigger foods, eating smaller meals, maintaining an upright posture after meals, and quitting smoking.
- Weight loss surgery: Losing weight, especially via a Roux en Y Gastric bypass, is an excellent way of reducing reflux.
Preparation Before Anti-Reflux Surgery
Before undergoing anti-reflux surgery, several preparatory steps are necessary. These may include:
- Medical Evaluation: A thorough medical evaluation will assess the individual's overall health, determine the severity of GORD, and rule out any underlying conditions.
- Pre-operative Instructions: Patients will receive specific instructions regarding dietary restrictions, medication management, and lifestyle modifications in the weeks leading up to the surgery. It is crucial to follow these instructions closely to ensure optimal surgical outcomes.
Anti-Reflux Surgery Procedure
Anti-reflux surgery is performed under general anaesthesia. Steps involved in the procedure include:
- Your surgeon makes five small incisions in the upper abdomen, inserting a telescope and several other instruments into the abdomen. The procedure is done by watching a monitor.
- The hole in the diaphragm through which the oesophagus passes is then tightened with sutures.
- Your surgeon wraps the upper part of the stomach (called the fundus) around the lower oesophagus to create a valve, suturing it in place.
- The laparoscope and other instruments are removed, and the gas is released.
- The tiny incisions are then closed.
What to Expect After Anti-Reflux Surgery?
After anti-reflux surgery, patients can expect the following:
- Hospital Stay: Most patients can expect to stay in the hospital for a day or two after the surgery to monitor their recovery and manage postoperative discomfort.
- Diet Progression: You will start with a liquid diet immediately postoperatively. You will go home on a puree diet for four weeks if tolerated. You can then gradually transition to solid foods as guided by your surgeon or dietitian.
- Recovery and Healing: It may take several weeks for the incisions to heal completely, and you should follow your surgeon's instructions regarding activity restrictions and wound care. Generally, the restrictions after this type of surgery are minimal.
Anti-Reflux Surgery Care Plan
Wound Care
- The small incisions are covered with waterproof dressings so you can shower.
- They should be removed after ten days.
Pain Management
- You may feel soreness around the incision areas. As (during the procedure), the abdomen was distended with gas.
- Your surgeon may prescribe pain medicine to keep you comfortable for the first few days.
- You may experience discomfort in the abdomen, chest, or shoulder area for several days.
Activity
- Shortly after surgery, you can gradually resume your daily activities.
- You are encouraged to start walking as early as possible to reduce the risks of blood clots and pneumonia.
- You are advised not to lift heavy objects (more than 3 kg) for six weeks.
Work
- You can get back to work in two to three weeks.
Anti-Reflux Surgery Outcomes
The outcome of treatment varies from person to person. Surgery is beneficial in approximately 90% of patients. Many patients who have suffered for years from heartburn and required medication to control the symptoms find that all symptoms are alleviated as soon as they awake from surgery and no longer need medication.
Anti-Reflux Surgery Risks
As with any surgical procedure, anti-reflux surgery carries potential risks and complications, including infection, bleeding, adverse reactions to anaesthesia, damage to surrounding structures, and post-operative discomfort. Fundoplication may involve certain side effects.
These can include trouble swallowing, inability to burp or vomit, bloating and passing more wind. These side effects do not occur in everyone. Patients should discuss these risks with their surgeons and be aware of the potential complications.






