Gallbladder Disease
What is the Gallbladder?
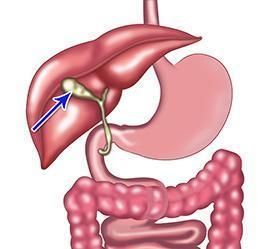
The gallbladder is a small, pear-shaped organ under your liver on the right side of your abdomen. It plays a vital role in your digestive system by storing and concentrating a digestive fluid called bile. It is immediately adjacent to the bile duct and closely related to the pancreas.
What are Gallstones?
Gallstones are hardened, pebble-like material that can form inside your gallbladder. They are usually composed of cholesterol, bilirubin, or both. While some people may not experience any symptoms from gallstones, others can suffer significant discomfort and complications. Once you have experienced gallstone symptoms, the treatment usually involves removing the gallbladder.
Gallstones usually range from a grain of sand (sometimes called sludge) to 3-4 cm. They can grow to fill the gallbladder virtually.
Types of Gallstones:
- Cholesterol stones
- Pigment stones
- Mixed stones
Risk factors for Gallstones
Some factors increase your chances of developing gallstones:
- Gender - Gallstones are more common in women
- Age - Gallstones are rarer in children than adults
- Genetics - Some families are genetically predisposed to developing gallstones
- Obesity - Especially in women.
- Rapid weight loss - As the body metabolises fat during rapid weight loss, it causes the liver to secrete extra cholesterol into bile.
- Oestrogen - Excess oestrogen from pregnancy, hormone replacement therapy, or birth control pills.
- Diabetes - People with diabetes generally have high levels of fatty acids called triglycerides.
Symptoms of Gallstones
Many people have gallstones but don’t have any symptoms associated with them. Only in specific circumstances would your surgeon suggest removing the gallbladder for ‘silent’ gallstones.
Symptoms, when they do occur, often follow fatty meals or occur at night.
Typical symptoms include:
- Pain in the upper and right side of the abdomen. Often, this pain can be quite severe and last for hours. Sometimes, this pain is felt in the chest or the back.
- There are less typical symptoms, like nausea and bloating, which might be associated with gallstones. Your surgeon will always take care to figure out if your symptoms are likely to be related to gallstones.
An accurate diagnosis is important to decide which treatment best suits your problem.
Gallbladder Disease
Often, gallstones do not cause any problems, but if gallstones block the gallbladder outlet, trapping the bile in the gallbladder, pain and inflammation can result.
Gallstones are responsible for the majority of gallbladder diseases. Gallstones may lead to gallbladder inflammation, known as acute calculous cholecystitis. Other less common conditions can also develop as a result of gallstones.
Some other gallbladder diseases include
- Bile duct stones (choledocholithiasis)
- pancreatitis
- gallbladder polyps
- gallbladder cancer
Bile duct infections and pancreatitis can lead to serious illness if not treated.
With prompt diagnosis and treatment, the outcome is excellent.
Diagnosis of Gallbladder Disease
Your GP or surgeon may use various tests to determine whether you have a condition related to your gallbladder or bile duct. Some of these tests find structural issues, like the presence of gallstones, while other tests examine the gallbladder's function. These tests might include:
- Blood tests
- Ultrasound
- Computed tomography (CT)/MRI are used in specific circumstances.
- HIDA scan
What is Gallbladder Surgery?
Gallbladder surgery, also known as cholecystectomy, is the surgical process of removing the gallbladder. This procedure is commonly advised for treating gallstones that cause symptoms. Additionally, it's used to address other conditions like biliary dyskinesia, which is an abnormal emptying of the gallbladder and gallbladder polyps.
Almost always, this surgery is carried out using a laparoscopic approach, also known as keyhole surgery. This minimally invasive method reduces discomfort and a shorter hospital stay. It may be appropriate for some patients to go home on the same day as their surgery.
During the procedure, additional diagnostic or therapeutic steps might be taken. This can include a cholangiogram, an intraoperative X-ray procedure used to define the anatomy of the bile ducts clearly and to check for the presence of any stones. In some cases, if gallstones are found within the bile ducts, a common bile duct exploration might be performed to remove these stones.
Who is a Candidate for Gallbladder Surgery?
Gallbladder surgery is typically recommended for individuals with gallstones or complications related to these gallstones. The following are common situations where gallbladder surgery may be considered:
- Gallstones: If you have gallstones causing symptoms such as abdominal pain, nausea, vomiting, or jaundice, your surgeon may recommend gallbladder surgery.
- Cholecystitis refers to gallbladder inflammation, often due to gallstones blocking bile flow. Acute cholecystitis can cause severe pain, fever, and abdominal tenderness.
- Biliary dyskinesia: Some individuals may have a gallbladder that doesn't function properly, known as biliary dyskinesia. It can lead to symptoms similar to gallstones, such as abdominal pain and indigestion.
- Gallbladder polyps: Polyps are abnormal growths that can develop in the gallbladder. While most gallbladder polyps are benign, some may have the potential to become cancerous.
- Choledocholithiasis occurs when gallstones migrate from the gallbladder and become lodged in the common bile duct, which carries bile from the liver to the small intestine. If the stones cannot be removed through nonsurgical techniques, surgery may be required to remove the gallbladder and the stones from the common bile duct.
Your surgeon will consider your symptoms, medical history, and overall health to determine whether gallbladder surgery suits you.
Benefits of Gallbladder Surgery
Gallbladder surgery offers several benefits for individuals with gallbladder conditions. Some of the key benefits include
- Relief from symptoms: Gallbladder problems, such as gallstones or inflammation, can cause significant pain and discomfort. Gallbladder surgery relieves these symptoms, eliminating the source of the problem.
- Prevention of complications: Gallbladder conditions can lead to complications if left untreated. For example, untreated gallstones can block the bile ducts, causing inflammation, infection, or even pancreatitis. By removing the gallbladder, the risk of these complications is eliminated.
Types of Gallbladder Surgery
There are two main types of gallbladder surgery:
- Laparoscopic cholecystectomy: This is the most common method used for gallbladder removal. It involves making several small incisions in the abdomen and inserting a laparoscope (a thin, flexible tube with a light and camera) to guide the surgical instruments. The surgeon then removes the gallbladder using specialised tools. Laparoscopic cholecystectomy is minimally invasive, resulting in smaller incisions, less scarring, and shorter recovery times.
- Open cholecystectomy: If complications are encountered or laparoscopic surgery is not possible, an open cholecystectomy may be performed. This involves making a larger incision in the abdomen to access and remove the gallbladder directly. Open cholecystectomy generally requires a longer recovery period compared to laparoscopic surgery. This is only very rarely performed.
Preparation Before a Gallbladder Surgery
Before undergoing gallbladder surgery, there are several important steps and preparations to follow. Here are some general guidelines:
- Consultation: Schedule a consultation with your surgeon to discuss the procedure, potential risks, and benefits. They will evaluate your medical history, perform a physical examination, and may order diagnostic tests.
- Preoperative instructions: Follow specific preoperative instructions provided by your surgeon. These may include dietary restrictions, medication adjustments, and guidelines on fasting before the surgery.
- Preoperative testing: Undergo any necessary preoperative tests, such as blood work, imaging scans, or electrocardiogram (ECG), to assess your health and ensure you are ready for surgery.
- Fasting: Follow instructions on fasting, which typically involves not eating or drinking anything for a certain period before the surgery. This reduces the risk of complications during anaesthesia.
- Transportation arrangements: Arrange for someone to accompany you and drive you home after the surgery, as you will be under anaesthesia.
What Happens During a Gallbladder Surgery?
During gallbladder surgery, the surgeon will perform the following steps:
- Anaesthesia: Receive general anaesthesia to be in a deep sleep without pain.
- Incisions: The surgeon will make small incisions in your abdomen, typically using laparoscopic techniques. These incisions allow access for instruments and a laparoscope (a camera on a flexible tube) to visualise the surgical area.
- Cholangiogram: Your surgeon will perform a cholangiogram during your operation to check if any gallstones have moved from your gallbladder into the bile duct.
- Removal of the gallbladder: The surgeon detaches the gallbladder from the liver and bile ducts, which are then removed through one of the incisions.
- Closure: The incisions are closed with absorbable sutures under the skin. There won’t be any need for sutures to be removed post-operatively.
What to Expect After a Gallbladder Surgery?
After gallbladder surgery, you will be taken to a recovery room, where you will be monitored until you wake up from anaesthesia. Depending on the type of surgery, you may be discharged on the same day or within a day or two.
Gallbladder Surgery Recovery
After gallbladder surgery, following a well-planned recovery plan can help ensure a smooth and successful healing process. While every individual's recovery may vary, here are some general guidelines for a gallbladder surgery recovery plan:
- Rest and recovery: Follow your surgeon's advice on how much rest you need and gradually increase your activity levels as you feel able to.
- Pain management: Take the medication as prescribed and as needed, following the instructions provided by your healthcare provider. Often, the pain is minimal.
- Incision care: Keep the incision sites clean and dry as instructed by your surgeon.
- Diet and eating habits: Initially, you may be advised to follow a low-fat diet to allow your body to adjust to the absence of the gallbladder. Gradually introduce regular foods as tolerated, and listen to your body's cues regarding what foods may cause discomfort or digestive issues.
- Physical activity: Initially, focus on gentle activities such as short walks, gradually increasing the duration and intensity as your surgeon advises.
- Medication management: If prescribed medications, such as antibiotics or pain medications, continue taking them as directed. If you have any concerns or experience side effects, consult your surgeon.
- Follow-up appointments: Attend all scheduled follow-up appointments with your surgeon. These appointments are important for monitoring your recovery, checking results, and addressing concerns or questions.
- Gradual return to normal activities: Gradually resume your normal activities, including work, as you can and as your surgeon advises. Listen to your body and avoid pushing yourself too quickly. It's important to give yourself enough time to recover fully.
Gallbladder Surgery Outcomes
The outcomes for gallbladder surgery are generally excellent. The surgery is a common and well-established procedure with a high success rate. Most people experience relief from the symptoms that led to the surgery and can resume their normal activities after recovery.
Gallbladder Surgery Risks
Gallbladder surgery is an exceedingly safe and commonly performed procedure. However, like any surgery, it does carry certain risks. It's important to be aware of these potential risks and discuss them with your surgeon before deciding on surgery. Some of the risks associated with gallbladder surgery include:
- Infection: There is a risk of infection at the incision sites or within the abdominal cavity. Precautions are taken to minimise this risk, such as using sterile surgical techniques and prescribing antibiotics when necessary.
- Bleeding: There is a small risk of bleeding during or after surgery. Your surgeon will take steps to minimise bleeding; if excessive bleeding occurs, it may require further intervention.
- Injury to surrounding structures: There is a slight risk of accidental injury to nearby structures during surgery, such as the bile ducts, liver, or intestines. Surgeons take precautions to minimise the risk of such injuries, but they can still occur in rare cases.
- Adverse reaction to anaesthesia: General anaesthesia carries risks, including allergic reactions, respiratory problems, or adverse reactions to the medications used. Anaesthesia-related risks are typically minimised by thorough preoperative evaluation and monitoring during surgery.
- Conversion to open surgery: In rare cases, a laparoscopic cholecystectomy may need to be converted to open cholecystectomy during surgery due to unforeseen circumstances or complications. This involves making a larger incision, resulting in a longer recovery time and increased risk of complications.
The risks associated with gallbladder surgery are generally low. However, the specific risks for an individual can vary based on factors such as overall health, the presence of any underlying medical conditions, and the complexity of the procedure.






